Effective communication between doctors and patients is critical to high-quality care, but it’s also one of the most strained aspects of modern healthcare. Clinicians are under constant pressure to document every visit detail while maintaining eye contact, listening closely, and responding thoughtfully. The result is a growing gap between patient expectations and clinical reality.
A study published in Health Affairs revealed that for every hour doctors spend with patients, they spend nearly two additional hours on documentation. This reduces face-to-face time, fragmented conversations, and increased burnout among healthcare professionals.
The consequences extend beyond the clinician’s well-being. Patients often leave appointments feeling unheard or rushed. Significant symptoms may be missed, details can be forgotten, and follow-up care suffers from incomplete documentation.
This is where AI-driven real-time medical transcription is making a measurable difference.
AI tools for healthcare are now being used to transcribe, summarize, and organize clinical conversations as they happen, without interrupting the flow of patient care. By replacing manual note-taking with real-time, AI-supported transcription, healthcare providers are solving one of the most persistent problems in clinical settings: maintaining accurate records without compromising real human connection.
This blog will explore how this technology works, its real-world impact, and why it’s becoming essential to the future of healthcare delivery.
How Does Real-Time Transcription Work in Healthcare?
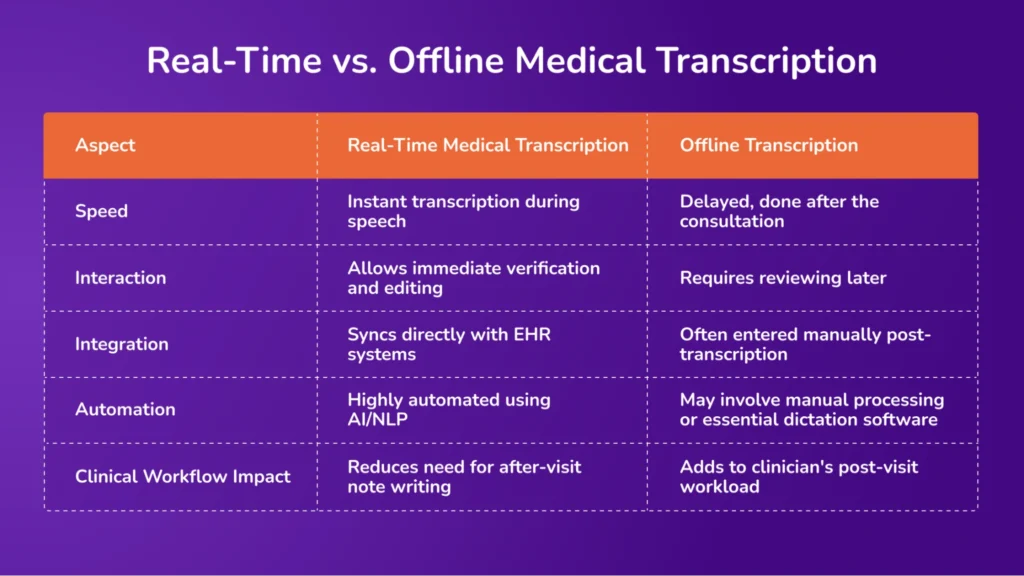
Real-time medical transcription (RTMT) converts spoken medical language into written text immediately after it is spoken. It is commonly used during clinical consultations, allowing healthcare providers to generate documentation while interacting with patients.
How It Works
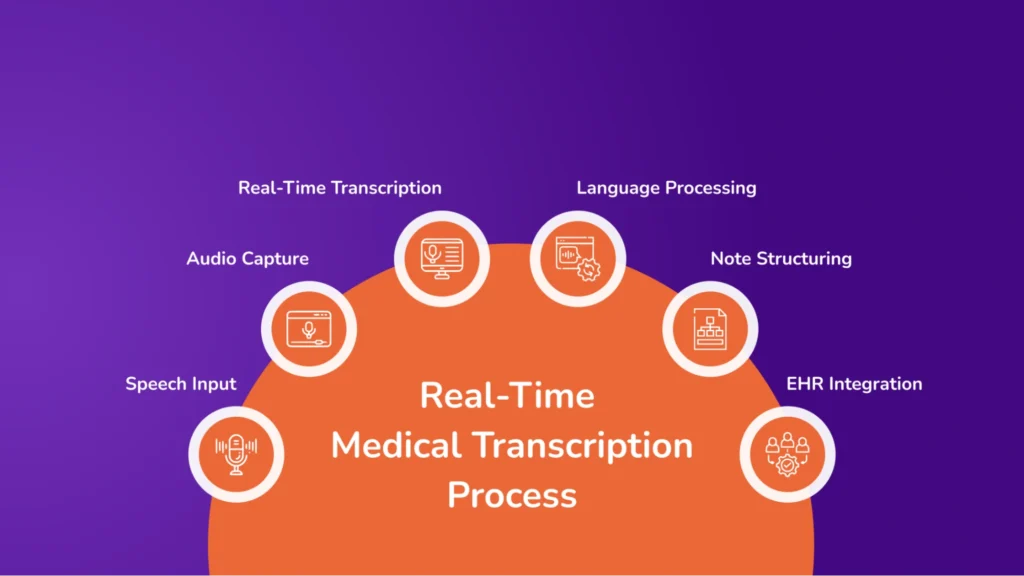
The clinician speaks or uploads an audio during a patient interaction. The voice input is captured through a microphone or device. The system uses AI-powered speech recognition to convert speech into text in real time. Medical NLP interprets medical terms, abbreviations, and context. The generated text is formatted and optionally integrated directly into the patient’s electronic health record (EHR).
Components of Real-Time Medical Transcription
The process relies on advanced technologies such as speech recognition, natural language processing (NLP), and cloud computing to deliver accurate, structured medical text without delay. This enables clinicians to reduce manual documentation time and focus more on patient care. Here is the explanation of each of these AI technologies:
Voice Recognition Software
Voice recognition software listens to a healthcare provider’s spoken words and converts them into written text. This process depends on two essential technologies: acoustic modeling and language modeling.
Acoustic modeling analyzes the unique sound patterns of speech, helping the system recognize different accents, speech speeds, and pronunciations. Language modeling predicts likely word sequences based on grammar, syntax, and medical context, improving the transcribed output’s accuracy. Well-known platforms such as Amazon Transcribe Medical provide this functionality.
Medical Natural Language Processing (NLP)
Once the speech is converted into text, medical natural language processing (NLP) interprets and organizes the content to reflect clinical relevance. NLP systems are trained to understand medical terminology, abbreviations, and context-specific phrases.
They perform entity recognition, which means they can identify critical clinical elements such as symptoms, diagnoses, procedures, and medications. In addition, they analyze the context of a sentence to determine its meaning, helping avoid misinterpretations. This makes the transcribed content more usable for medical documentation and decision-making.
Cloud-Based Systems
Cloud computing allows for processing large volumes of audio and text data without the need for local infrastructure. Through cloud-based systems, transcription services can operate on demand and scale as needed, offering real-time data streaming and storage.
These systems also provide encrypted data handling to meet healthcare privacy requirements. Cloud platforms allow clinicians to access transcription services across multiple devices and locations, improving flexibility and efficiency.
Electronic Health Record (EHR) Integration
For transcription to be helpful in a clinical setting, it must integrate directly with electronic health record (EHR) systems. This integration ensures that the transcribed text becomes part of the patient’s official medical record without requiring additional manual input.
EHR integration typically relies on standardized protocols like HL7 or FHIR (Fast Healthcare Interoperability Resources) to enable secure and structured data exchange. It also supports workflow automation, allowing clinical notes to be tagged, categorized, and routed to the appropriate sections of the health record. This improves accuracy and reduces the administrative burden on healthcare providers.
Benefits of AI Medical Transcription Across Global Healthcare
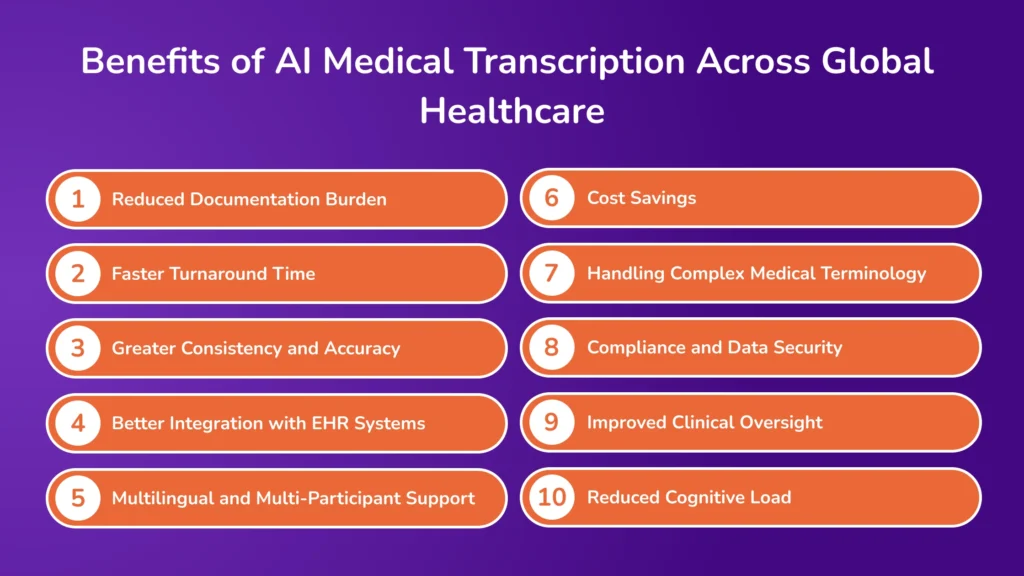
According to recent industry data, AI note-taking solutions can cut documentation time by up to 50% and improve transcription accuracy to 90% or higher, even across multiple languages. Below is the list of significant ways AI transcription is driving this transformation:
1. Reduced Documentation Burden
Physicians spent an average of 16 minutes per patient on documentation. A 2024 study published in JAMA Network Open found that 47.1% of clinicians using AI documentation reported decreased time on EHR documentation at home, and 44.7% reported reduced documentation time outside regular work hours.
AI transcription tools automate medical note-taking in real time, reducing the time needed for charting by several minutes per patient. Over a day, this leads to hours saved. These tools improve physician satisfaction and care quality by shifting the focus back to patient care and away from clerical work.
2. Faster Turnaround Time
Regular documentation processes often involve delays between seeing patients and completing their records. Real-time transcription removes that lag by instantly converting spoken notes into structured clinical text.
For example, the Permanente Medical Group adopted ambient AI tools for over 10,000 clinicians in 2023. Within ten weeks, providers reported reduced time spent in electronic health records (EHRs) after hours and more focused patient interactions. Clinical teams can review, act on, and share documentation without delay, speeding up follow-ups, referrals, and treatment adjustments.
3. Greater Consistency and Accuracy
Manually written notes can vary in detail and structure, especially under time pressure. Real-time transcription creates standardized documentation, reducing inconsistencies. A recent study found that AI-assisted documentation tools reduced variability in clinical notes and improved the consistency of symptom reporting across providers. Uniform records improve care continuity and make it easier for teams to interpret patient history across departments or providers.
4. Better Integration with EHR Systems
Real-time transcription tools often have built-in EHR compatibility or support easy data transfer. Clinicians can quickly plug generated notes into existing workflows without extra steps.
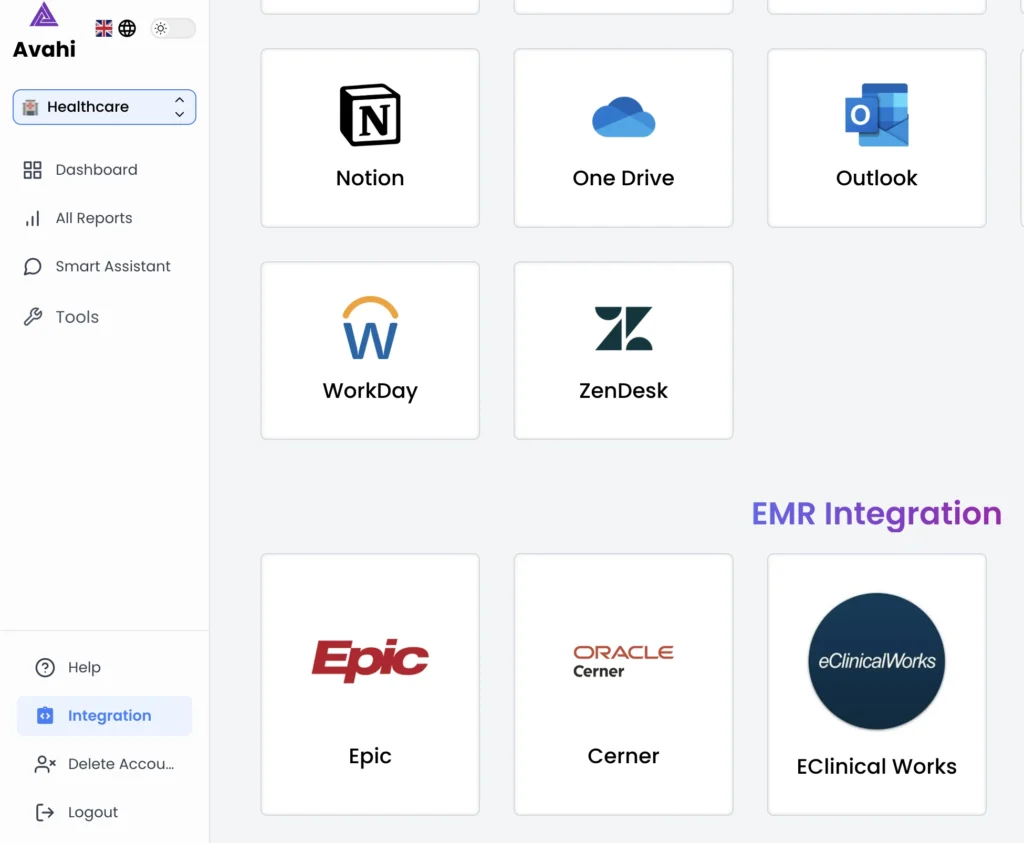
AI transcription systems are integrated directly into leading Electronic Health Record (EHR) platforms like Epic, Oracle Health, and eClinicalWorks. This means notes are transcribed and automatically updated in the patient’s digital chart without requiring manual entry. The result is cleaner records and faster data access for healthcare teams. Providers reduce the time spent formatting or re-entering notes, minimizing duplicate work and system friction.
5. Multilingual and Multi-Participant Support
Modern transcription tools now support multiple languages and recognize more than one speaker, especially in group settings or diverse populations. This improves inclusivity and documentation accuracy in multilingual environments and group consults, enhancing patient understanding and safety.
6. Cost Savings
AI transcription reduces reliance on manual scribes or third-party transcription services, which can be expensive and time-consuming. According to insights from the Augmented Intelligence for Healthcare Operations report, AI-powered solutions are helping healthcare organizations improve efficiency and reduce operational costs. AI tools help to lower overhead costs and scale documentation efforts without hiring more staff.
7. Handling Complex Medical Terminology
Modern AI systems are trained on vast datasets of clinical conversations, enabling them to recognize medical vocabulary across dozens of specialties. These tools also understand the context behind terms, helping differentiate between similarly sounding conditions or medications and supporting accurate record-keeping.
8. Compliance and Data Security
AI transcription platforms have built-in compliance features to meet strict regulations like HIPAA and GDPR. These include encryption, user-level access controls, and audit trails.
A study found that speech recognition reduced documentation time from 8.9 to 5.1 minutes per task while decreasing error rates. These improvements help healthcare systems maintain accurate records while complying with data protection laws.
9. Improved Clinical Oversight
Real-time transcription tools often include automatic time stamps, speaker labels, and audit-ready logs. This makes it easier to trace and validate care decisions when needed.
AI platforms integrated into large health systems often store metadata like who spoke, when, and which portions of a note were auto-generated or manually edited. This helps to strengthen legal compliance, quality assurance, and training opportunities, especially in complex or high-risk specialties.
10. Reduced Cognitive Load
When doctors don’t need to remember details for post-visit documentation, they can focus more clearly on the patient and clinical decision-making. Fewer distractions during care delivery lead to better decisions, less fatigue, and improved patient outcomes.
Challenges of Manual Medical Documentation in Healthcare
Manual and outdated documentation methods are a growing problem in modern healthcare. They slow clinical workflows, introduce errors, and reduce clinicians’ time with patients. Below are six significant challenges that healthcare providers face with manual documentation systems.
1. Time-Intensive and Disruptive Workflows
Healthcare providers spend a significant portion of their day completing notes and entering data into records. This slows down operations and reduces the time available for patient care.
Manual note-taking during or after appointments interrupts clinical flow. Routine paperwork takes up hours of provider time each week, forcing many clinicians to work beyond scheduled hours to finish documentation.
2. Delays in Transcription
The conventional transcription process, recording, transcribing, reviewing, and approving, adds time before notes are finalized and usable. This slows down care coordination and decision-making.
Turnaround times can range from several hours to a full day. Delays in documentation affect referrals, diagnoses, and treatments. Workflow backlogs and staff shortages increase the risk of bottlenecks.
3. Reduced Patient Engagement
Documentation during appointments often distracts providers from giving patients their full attention, affecting rapport and trust in the patient-provider relationship.
Divided focus limits the quality of communication. Lack of eye contact or active listening may impact patient satisfaction. Patients may feel overlooked when notes take priority during the visit.
4. Risk of Clinical Errors and Miscommunication
Manual documentation is prone to errors. These mistakes can lead to incorrect treatment, duplicate testing, or missing vital information in the patient’s record.
Human error in transcription or data entry can affect care decisions. Inconsistent or incomplete records disrupt follow-up plans, and illegible handwriting or ambiguous notes can lead to misinterpretation.
5. High Administrative Burden and Staff Burnout
The administrative load tied to traditional documentation contributes to burnout among clinicians. Constant documentation pressure reduces job satisfaction and increases turnover risk.
Clinicians report stress from balancing documentation and patient care. Extended hours for charting negatively impact work-life balance, and burnout affects care quality, team morale, and retention.
6. Limited Flexibility and Scalability
Manual documentation systems don’t scale well as patient volumes increase. They also struggle to adapt to new digital workflows and integrated care systems.
Growing documentation needs create pressure on limited staff resources. Manual processes can’t easily support remote care or telehealth expansion, and inflexible systems make adopting innovations like AI or automation harder.
Avahi AI Platform Features: Built for Smarter Clinical Workflows
The AvahiAI Platform offers a powerful medical scribing feature to automate and streamline clinical documentation. Here’s how it works within your workflow:
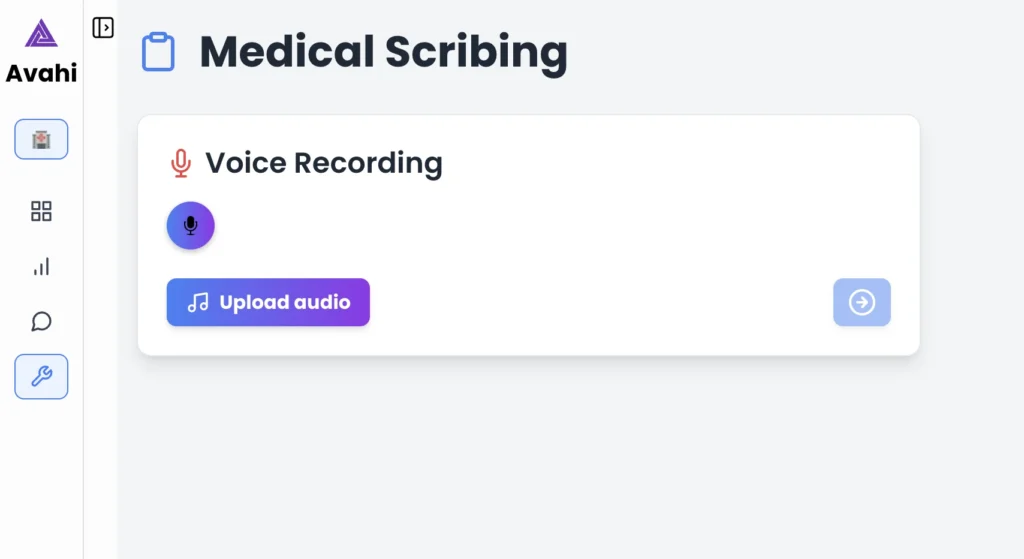
1. Real-Time Transcription (Live or Uploaded)
AvahiAI supports both live transcription during consultations and transcription from uploaded audio or video files. Users can simply drag and upload a recorded video of a patient encounter, and the system will begin transcribing it immediately.
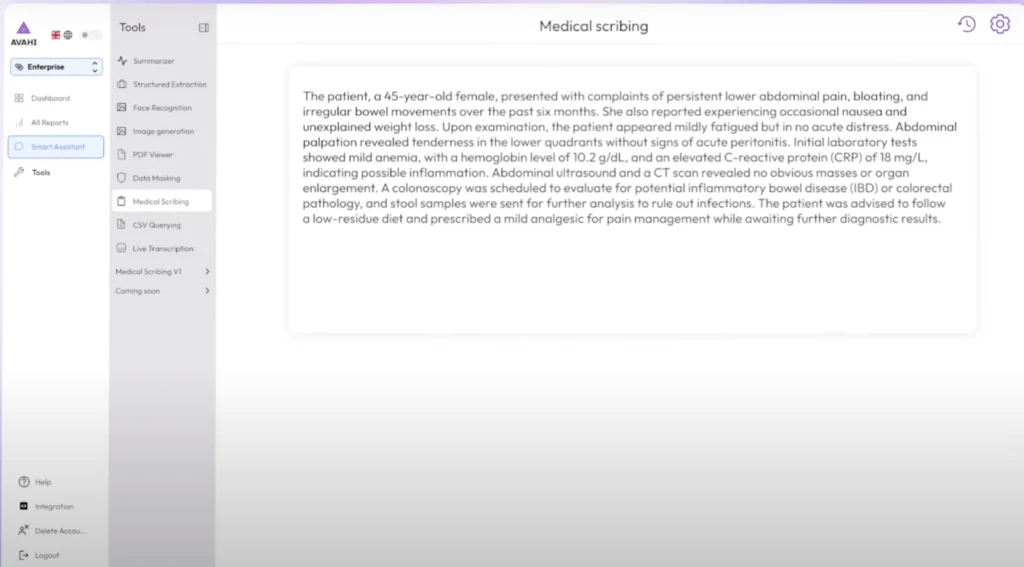
Whether you’re speaking in real time or uploading a session for later processing, the AI captures the content with high accuracy and generates a structured clinical note by the end of the session.
2. Speech Recognition During Patient Visits
AvahiAI listens during patient consultations or while you dictate notes. Using advanced medical speech recognition, it captures spoken words accurately and converts them into structured text. The system is built to understand medical terminology, abbreviations, and clinical context.
3. Adapts to Your Style and Specialty
AvahiAI learns your preferred documentation style, commonly used phrases, and specialty-specific language. Over time, it delivers clinical notes that reflect your voice and structure, requiring fewer edits.
4. Easy Review and Edits
Once the initial transcription is done, you can review, edit, and approve the note. The platform highlights any uncertain sections for quick verification. The edits will further improve accuracy and personalization in future sessions.
5. EHR-Ready Output
Finalized notes can be easily transferred to your Electronic Health Record (EHR) system using simple copy/paste or direct integration. This helps reduce manual entry and ensures accurate, timely patient records.
Why Choose AvahiAI for Medical Scribing and Documentation?
The Avahi AI Platform is made to streamline healthcare workflows by automating real-time medical documentation. Built-in medical scribing capabilities help providers capture accurate clinical notes during patient interactions.
Accurate Medical Documentation
AvahiAI is trained on diverse clinical datasets to understand and transcribe complex medical language, including diagnostic terms, treatment plans, and patient history. It significantly reduces errors in medical notes by accurately recognizing context-specific terminology.
Time Savings for Clinicians
By automating note-taking, AvahiAI helps providers save significant time on documentation. This allows them to focus more on patient care and less on administrative tasks, reducing cognitive load and burnout.
Support for Diverse Accents
AvahiAI is trained to understand various accents and region-specific clinical terms, making it effective in diverse healthcare environments, including large hospitals and distributed telehealth setups.
Customizable for Specialized Use Cases
Healthcare organizations can fine-tune the scribing engine to recognize specialty-specific language or adapt it for custom workflows, such as surgical notes, mental health sessions, or pediatric care.
Discover Avahi’s AI Platform in Action
At Avahi, we empower businesses to deploy advanced Generative AI that streamlines operations, enhances decision-making, and accelerates innovation—all with zero complexity.
As your trusted AWS Cloud Consulting Partner, we empower organizations to harness AI’s full potential while ensuring security, scalability, and compliance with industry-leading cloud solutions.
Our AI Solutions Include
- AI Adoption & Integration – Utilize Amazon Bedrock and GenAI to enhance automation and decision-making.
- Custom AI Development – Build intelligent applications tailored to your business needs.
- AI Model Optimization – Seamlessly switch between AI models with automated cost, accuracy, and performance comparisons.
- AI Automation – Automate repetitive tasks and free up time for strategic growth.
- Advanced Security & AI Governance – Ensure compliance, fraud detection, and secure model deployment.
Want to unlock the power of AI with enterprise-grade security and efficiency?
Get Started with Avahi’s AI Platform!